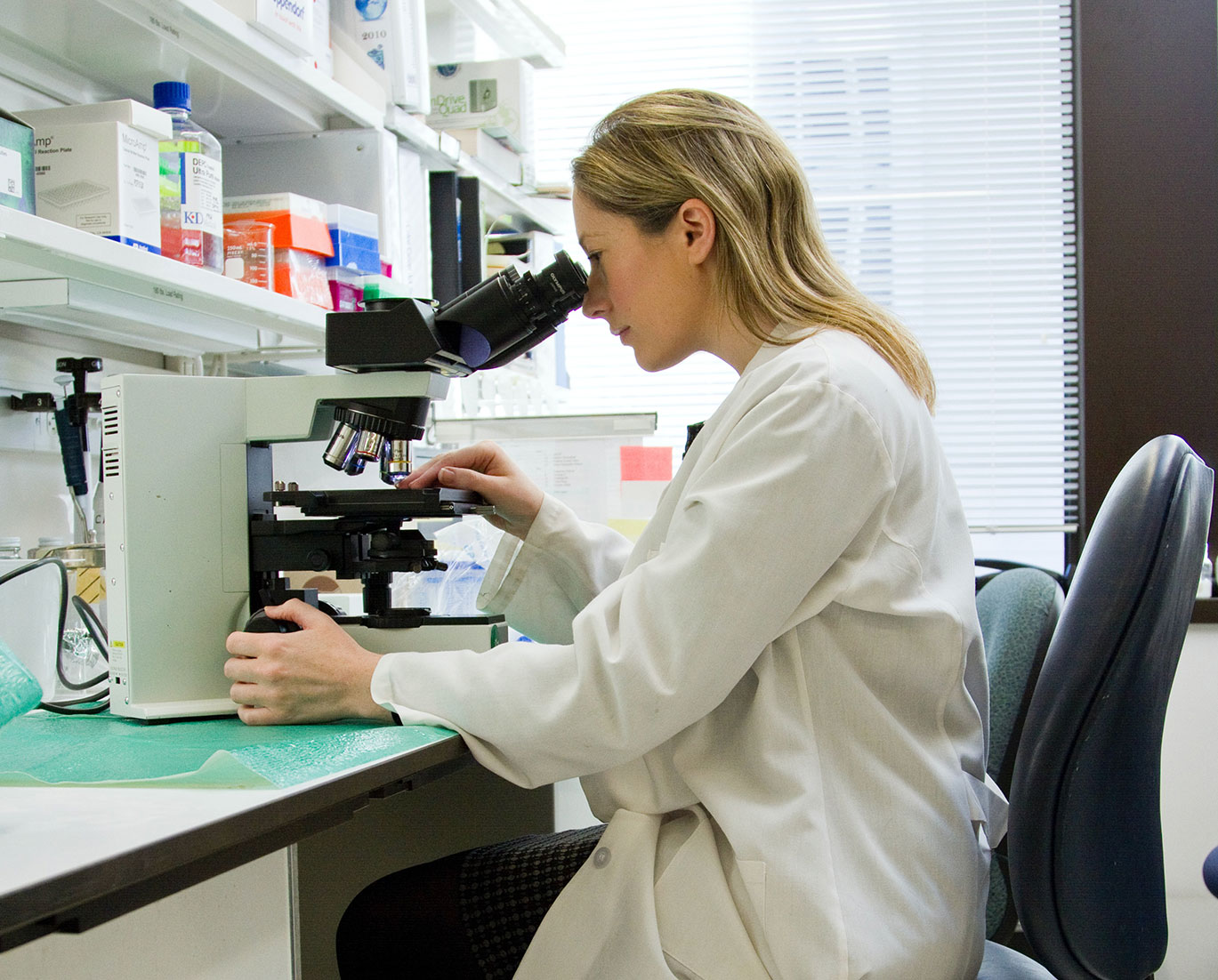
Om æggestokkræft
The Silent Killer
Kræft i æggestokkene kaldes også ’The Silent Killer’ fordi sygdommen har meget uspecifikke symptomer, der nemt kan forveksles med andre, mindre alvorlige, diagnoser. Derfor opdages sygdommen oftest for sent, dvs. når kræften har bredt sig og helbredelsesmulighederne er meget dårlige. Meget få bliver helbredt – og sådan bør det ikke være – der er brug for mere forskning til at helbrede kvinderne. Kræft i æggestokkene har en meget lav overlevelsesrate, og hvert år rammes 550 danske kvinder af sygdommen. Det svarer til 1,5 kvinder om dagen.[1]